- DZL
- Research
- DZL Academy
- News
- Service
Researchers of DZL shed some light on the various types of asthma: they analyzed lung collagen degradation and found a way to predict the course of an antibody therapy with omalizumab. The results have been published this month in the European Respiratory Journal.
Asthma is not one and same disease in every patient. It is many different diseases with similar symptoms in different patients. One important aim of DZL’s asthma research is to find endotypes – certain subgroups of patients that can be distinguished by the same underlying cellular mechanism. Finding these endotypes could improve the development of specific drugs that are exactly tailored to one patient’s needs.
The protein collagen is quite various as well. Its sub-forms are involved in forming skin, tendons, cartilage, ligaments, bones, blood vessels and internal organs. One of these collagen sub-forms – COL4A3 – occurs mainly in lungs, esophagus and kidneys. Researchers found earlier that COL4A3 is reduced in pulmonary tissue of asthmatics due to inflammation and disturbed remodeling processes.
The new DZL study aimed at improving knowledge on degradation of COL4A3 in the airways of asthmatics. Therefore DZL scientists used biomaterial samples of the ALLIANCE registry as well as an animal model. Furthermore the researchers analyzed, if it is possible to forecast the process of an asthma therapy by measuring the degradation products of COL4A3 in the blood. Actually, the scientists identified higher levels of C4Ma3 – a degradation product of COL4A3 – in the blood of adult asthmatics compared to healthy control subjects. They found a dependency on the degree of severity of asthma and the occurrence of exacerbations (phases of disease aggravation). In children, asthma and C4Ma3 blood levels were interdependent, too.
Complementary study in mouse model
In order to study the mode of degradation of COL4A3, researchers switched to a mouse model. They obtained the same results in mice sensitized and challenged with ovalbumin or house dust mite: higher levels of C4Ma3 in the blood. Moreover, they measured higher levels of the enzyme mast cell chymase, which can degrade collagen. After inhalation of fulacimstat, an inhibitor of mast cell chymase, the degradation of COL4A3 decreased, but wasn’t completely suppressed. Thus, the DZL scientists assume that mast cell chymase is important for this process, although C4Ma3 can also accrue through a different degradation pathway.
Collagen degradation in clinical context
In allergic asthma, specific antibodies play a central role. They are produced after contact with the respective allergen, bind to mast cells and trigger the typical symptoms. Therapeutically, this type of asthma can be treated with another antibody: e. g. omalizumab. Omalizumab captures allergen-specific antibodies and prevents mast cell activation.
The central clinical question of the study was: How does the blood concentration of C4Ma3 change when patients with acute asthma are treated with omalizumab? The DZL researchers identified two groups: individuals who benefited from therapy and reported an improvement of symptoms, and persons without any change of symptoms. Interestingly, both groups could be differentiated on the basis of the C4Ma3 level: There was a significant decrease in blood C4Ma3 concentration of asthmatics which benefited from therapy. For persons who didn’t benefit, the level of C4Ma3 didn’t decline. This means that a high initial C4Ma3 level can predict the success of omalizumab therapy.
“The remodeling processes in the asthmatic lung can provide an excellent biomarker,” says study leader Dr. Markus Weckmann from the University Medical Center Schleswig-Holstein (UKSH) in Lübeck. “In this particular case, mast cell enzyme activity and organ-specific collagen ideally come together, which allows for better assessment of efficacy of therapy, even before starting it.” In addition, the researchers have succeeded in discovering a previously unknown endotype. The asthma of these patients shares the same cellular mechanism.
20 patients have been included in the omalizumab study. To get more robust results, the study will be repeated with a larger number of study subjects.
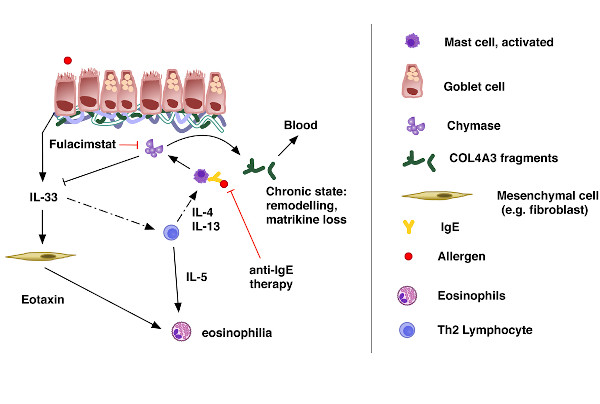
Mechanism of collagen degradation in allergic asthma according to Weckmann et al., European Respiratory Journal 2021 [M]
Above: Lung epithelium with underlying collagen layer
ALLIANCE is success story of the DZL
This project is a collaboration of the DZL sites ARCN, BREATH and CPC-M as part of the ALLIANCE asthma registry, one of the central projects of the Disease Area Asthma & Allergies. ARCN partners involved were UKSH, LungenClinic Grosshansdorf and Research Center Borstel. The authors published their results this month in the European Respiratory Journal.
Further information:
Original publication: COL4A3 is degraded in allergic asthma and degradation predicts response to anti-IgE therapy